I am officially a candidate for the Arizona House in Legislative District 1, which consists of most of Yavapai County plus the Sedona area. I am running with Jay Ruby and Mike Fogel on a Clean Slate for Democracy.
I am running to represent all residents of our District, not just those who agree with me. We are one community and we need legislators who will provide solutions to our problems, not ones who seek to divide us.
We all agree we need access to affordable healthcare. Arizona has a shortage of primary care practitioners. In Yavapai County, there is only one primary care physician for about 1,730 residents, many with high health care needs.
We need representatives who can effectively address this shortage so we can access healthcare when we need it. I understand the issues providers face and what policies can be adopted to help them help us.
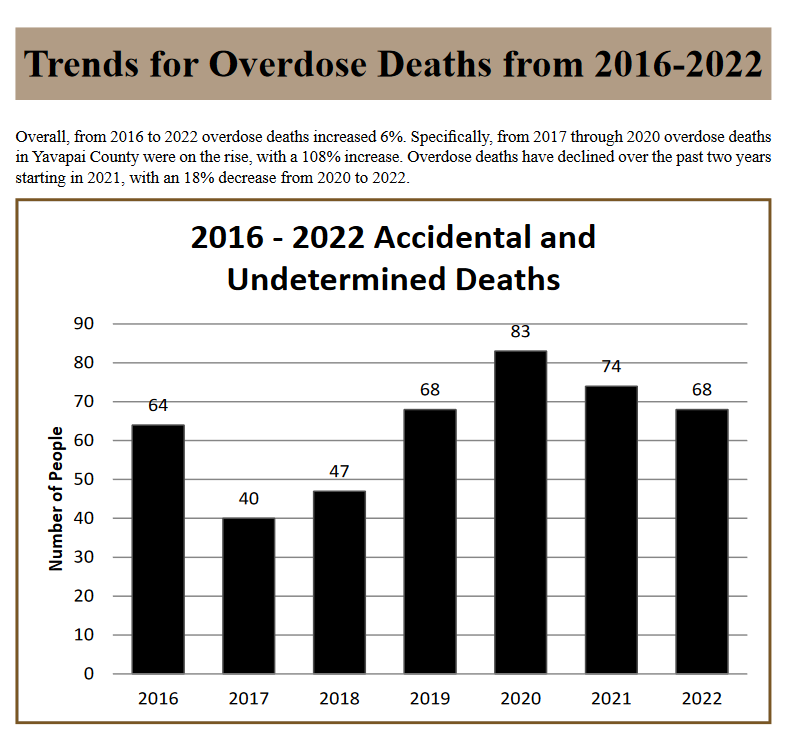
We can all agree our healthcare system must include mental health care resources to address the opioid overdose crisis and the epidemic of loneliness in our retirement communities. We need lawmakers who will ensure we have a robust community health system that includes all aspects of healthcare
Most of us agree women should have the right to make their own decisions about whether they are willing and able to continue a pregnancy. On April 8, 2024, Arizona’s Supreme Court issued a ruling restoring a law from 1864 that completely bans abortion across our state except in cases when it is necessary to save a woman’s life. This is an outrageous decision and is a direct result of the extreme agenda of MAGA Republicans like our opponents who are committed to taking our right to bodily autonomy.

If this law is not quickly repealed, pregnant women in Arizona will be denied life-saving healthcare because physicians will be too afraid to treat a pregnant woman if such treatment requires the termination of her pregnancy, even in cases where the mother’s life is at stake and the pregnancy is not viable. I support a women’s right to choose and the Arizona Abortion Access Act.
I am the youngest of 11 and grew up in Minneapolis in a working-class Catholic neighborhood where big families like mine were common. I graduated from the University of Minnesota, where I studied Economics and Spanish. I joined the Navy after college. After my Naval service, I attended Albany Law School. I have represented healthcare providers for over 25 years. My husband and I chose to live in Arizona because of its natural beauty and its commitment to individual liberty.



 Concerns Regarding Employment Model
Concerns Regarding Employment Model